Allergic reactions, which affect 30% of the world's population, and diseases such as rhinitis, asthma, urticaria/angioedema, and drug and food allergies, which are commonly seen as a result of these reactions, are significant public health problems that lower individuals' quality of life. The allergy and immunology medical unit carries out diagnosis and treatment practices for managing symptoms and disease processes associated with allergy and immune system disorders in adult patients.
What is Allergy and Immunology?
Allergy and immunology include clinical practices that aim to diagnose allergic reactions, plan their treatment, and manage immunodeficiency-related diseases.
Allergy is a mechanism that occurs when the immune system overreacts to a foreign substance that is usually harmless after a certain period of exposure. This condition, also known as hypersensitivity, can range from moderately discomforting symptoms to more severe and life-threatening systemic reactions. The type and severity of symptoms are related to how and to what extent the individual is exposed to the allergen and their sensitivity level. Urgent intervention is vital in patients developing severe systemic reactions.
Allergy and immunology specialists play an active role in preventing and treating the deterioration of quality of life, serious illnesses, and life-threatening reactions that can occur in allergic individuals, especially those who experience severe systemic reactions. Since pathological conditions associated with hypersensitivity to allergens can arise for different reasons, personalized approaches are applied for diagnosis, treatment, and reaction prevention.
What does the Allergy and Immunology Unit deal with?
Allergy and immunology specialists request the necessary tests and examinations to identify the triggering substance to prevent reactions that occur in allergic individuals. Depending on the allergen substance, one or more systems in the body may be affected. These reactions, which develop depending on the immune response, are more commonly observed in the skin and mucosal membranes, the outermost barriers against environmental factors. Developing sensitivity usually results in local inflammation. Increased histamine release in the body can increase mucus secretion in the nose and lungs, and allergic symptoms in the respiratory system can occur. The variety and intensity of the symptoms provide experts with a prediction for diagnosis. Diagnosis is made based on a detailed evaluation of the patient's complaints, history, and test results. The treatment process is planned by identifying allergens.
Common diseases treated in Allergy and Immunology Units include:
Allergic Rhinitis
Allergic rhinitis, which affects 10% to 30% of the world's population, results from inflammation of the nasal mucosa (non-microbial inflammation). Diseases that come with it include nasal polyps, sinusitis, conjunctivitis, middle ear infections, upper respiratory tract infections, and sleep disorders. Allergic rhinitis should not be neglected because it can trigger the development of asthma. Patients whose symptoms cannot be controlled with standard treatments (antihistamines, nasal steroids, etc.) must be evaluated by allergy and immunology specialists. Immunotherapy (desensitization treatment) in this patient group can significantly improve the patient's quality of life, reduce the need for medication, and prevent the progression of asthma.
Allergic Conjunctivitis
Allergic conjunctivitis affects over a million people worldwide and is the most common cause of eye redness. Allergens in the air can cause mild to moderate symptoms and, in some cases, lead to more severe inflammation involving the cornea. Therefore, it is among the allergic conditions that need to be controlled.
Asthma
Asthma is a chronic inflammatory respiratory disease that lasts throughout life. It is associated with airway obstruction and the overreaction of the respiratory tract to certain substances. Allergic asthma is often seen in atopic individuals who have a genetic predisposition to developing hypersensitivity to common allergens. It can negatively impact individuals' everyday activities and reduce their quality of life. Allergic asthma is a significant public health issue as it can lead to death if left uncontrolled. Correct treatment and follow-up of asthma can help control the disease and allow patients to live their daily lives without asthma-related issues. In 5-10% of asthma patients, standard treatments such as inhaled corticosteroids may not be sufficient to control asthma. In such cases, biological agent therapies administered by allergy and immunology specialists can significantly affect the patient's life.
Atopic Dermatitis (Eczema)
Atopic eczema, one of the most common chronic inflammatory skin diseases, manifests itself with various symptoms. In atopic individuals, redness and itching are generally the initial signs. The disease causes dysfunction of the epidermal barriers (the outermost layer of the skin) due to dry, flaky skin. This leaves the skin vulnerable to environmental allergens and affects the immune system.
Individuals who have had eczema since infancy are at high risk of developing allergic rhinitis and asthma later in life. The aim of treating those with atopic eczema is to prevent the development of other atopic diseases, control inflammation, and improve affected skin layers to increase their quality of life.
Urticaria
Urticaria, characterized by raised and reddish bumps (hives) on the skin, can be seen in acute (short-term) or chronic (long-term) forms. It is often seen acutely in food, drug, and insect allergies. However, a significant portion of acute urticaria occurs idiopathically (without an identifiable cause), and some cases of acute urticaria turn into chronic forms. In severe cases, it can result in angioedema. Allergy specialists should manage moderate and severe cases to bring the disease under control. At this stage, in addition to standard treatments (antihistamine and steroid therapy), biological agent therapies may also be considered by immunology and allergy specialists. It is known that these treatments significantly improve the patient's quality of life.
Food Allergy
Food allergy is a widespread problem that affects approximately 250 million people worldwide. Symptoms can range from mild to severe and can include atopic dermatitis, recurrent vomiting and diarrhea, hives, asthma attacks, and anaphylaxis. The reaction occurs when the individual consumes a food to which they are sensitive. The treatment involves identifying the allergen, removing it from the individual's diet, and providing them with adrenaline auto-injectors for protection. In some exceptional cases, desensitization therapy may be used in children, such as for selected cases of cow's milk allergy.
Drug Allergy
Adverse drug reactions usually occur as a result of unpredictable hypersensitivity and are responsible for over 20% of hospitalized patients. Common drugs that can cause allergic reactions include penicillin, cephalosporin, sulfonamide, aspirin, and other non-steroidal anti-inflammatory drugs (pain relievers). This type of allergy varies regarding the manifestation of symptoms, severity, and the organs affected. Early diagnosis and appropriate management of patients are crucial in drug allergies, as more than 20% of anaphylactic cases resulting from drug allergies lead to death. Alternative drugs to the allergenic drug should be identified through oral drug provocation tests. If there is no alternative or less effective drug than the allergenic one, desensitization treatment (immunotherapy) should be applied.
Bee Sting Allergy
Bee sting allergy, a common problem worldwide, can cause local or systemic allergic reactions in individuals. The developing allergic reaction can be limited to a local reaction at the sting site, such as redness, hives, and angioedema, or more severe symptoms may occur, such as bronchospasm, laryngeal edema, and low blood pressure. Diagnosis, treatment, and emergency interventions are essential, as these reactions can be fatal. Individuals with a bee sting allergy should undergo allergic evaluations. Immunotherapy (desensitization treatment) is a life-saving approach for individuals who have developed a systemic reaction.
Anaphylaxis
Allergic anaphylaxis is a life-threatening immune response that occurs primarily in adults after taking medication, eating certain foods, or being stung by insects and requires immediate intervention. The route of allergen exposure affects the severity and timing of the reaction. For example, symptoms may appear within seconds or minutes when medication is administered by injection, while with orally ingested drugs, symptoms may appear within a few minutes or even hours. In severe systemic reactions, anaphylaxis may lead to loss of consciousness or anaphylactic shock. Respiratory obstruction and cardiovascular collapse leading to arrhythmias may result in death.
Which Tests are Conducted in the Allergy and Immunology Unit?
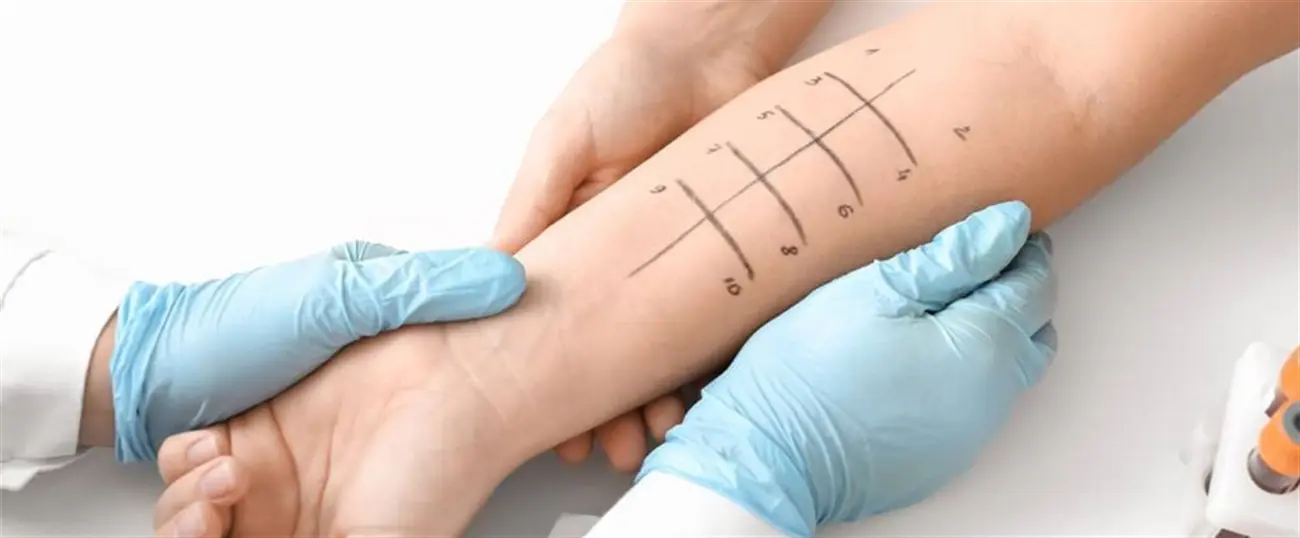
Avoiding allergens is the most effective and prioritized method for preventing allergic reactions. Therefore, it is necessary to identify the substances that stimulate the individual's immune system to overreact. Since most of the tests performed in this regard carry the risk of developing anaphylaxis to varying degrees, they are conducted under the supervision of experienced specialists. Sensitization in skin tests alone is not sufficient to diagnose an allergy. A comprehensive expert evaluation and the patient's clinical history are required to avoid false positive results.
The clinical practices performed for diagnostic purposes in the allergy and immunology unit are as follows:
- Skin tests: Prick Test, Intradermal Test, Patch Test
- Specific IgE Testing in Blood
- Respiratory Function Tests
- Reversibility Tests
- Bronchial Provocation Tests
- Drug/Food Provocation (Loading) Tests
The methods commonly used in the treatment of patients in the allergy and immunology unit are as follows:
- Pharmacological Treatment
- Immunotherapy and Desensitization Treatments
- Biological Agent Treatments.

 Let Us Call You
Let Us Call You