Endoscopy
Overview
Endoscopy, as a term, is an imaging method for organs with lumen.
In practice, endoscopy often refers to imaging the upper digestive tract (esophagus, stomach, and small intestines). For this reason, esophagogastroduodenoscopy is a medical term synonym for endoscopy.
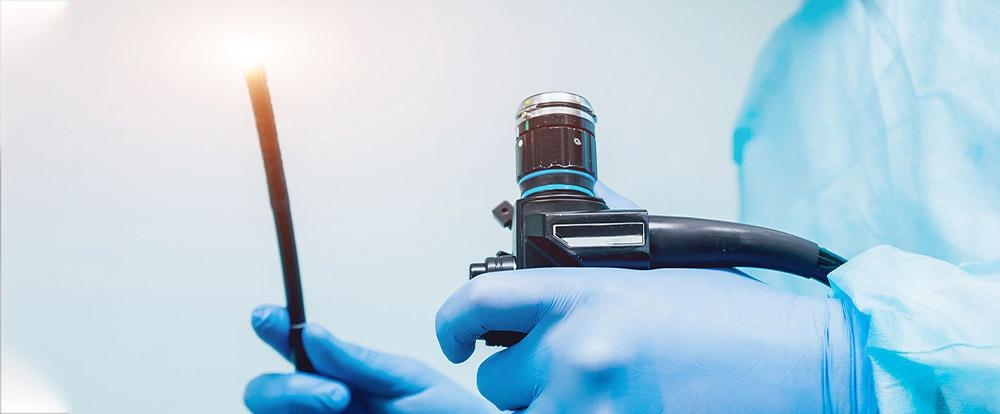
In endoscopy, a thin, flexible tube equipped with a camera, called the endoscope, is used. The endoscope is inserted into the oral cavity and advanced to the esophagus, stomach and small intestine, respectively. Meanwhile, the causes of symptoms possibly originating from the upper digestive system are investigated.
In endoscopy, a thin, flexible tube equipped with a camera, called the endoscope, is used. The endoscope is inserted into the oral cavity and advanced to the esophagus, stomach, and small intestine. Meanwhile, the causes of symptoms possibly originating from the upper digestive system are investigated.
Why is this procedure done?
Endoscopy is performed to directly visualize the upper digestive tract of patients, who present with upper gastrointestinal complaints (abdominal pain, cramp, difficulty swallowing, changes in bowel habits, stomach ache and dyspepsia) and patients with suspicious findings on stool analyses, laboratory tests and X-rays.
While the upper digestive system is examined, the gastroenterologist investigates the causes of active complaint as well as other possible pathologies. As the case for colonoscopy, endoscopy also allows both diagnosis and treatment.
Possible abnormalities of the upper digestive tract include, but not limited to abnormalities that can cause difficulty swallowing, bleeding, ulcers, inflammation, abnormal tissue changes, foreign bodies, narrowing, and cancerous formations.
Risks
It is rare to face a complication in the endoscopic examination of the upper digestive tract, and they are usually easily managed, even if they develop. Drug reactions and bleeding at the biopsy site are the most common ones. The perforation of the digestive tract examined with an endoscope is an infrequent complication.
All necessary instruments, equipment, and other means to manage the possible risks and complications are available in the endoscopy room.
Our specialists will employ all practices to minimize the risk of complications, and our doctors will inform you about the risks listed above and all other potential complications. They will address all your concerns before the procedure.
Preparation
Digested food in the esophagus, stomach, and the first part of the small intestine will jeopardize the quality of the upper GI endoscopy.
Since endoscopy is an elective (planned) procedure, you will be asked to stop eating and drinking eight hours before the procedure.
At the preparation phase, you need to notify all prescription and over-the-counter medications that you take to manage diabetes mellitus, hypertension, high blood lipids and cholesterol as well as other diseases and all vitamin and mineral supplements to your doctor. Your doctor will instruct medications that you should stop taking by consulting you with other specialist of our hospitals. Or, dose of those medications can be modified.
Since endoscopy is an elective (planned) procedure, you will be asked to stop eating and drinking eight hours before the procedure.
At the preparation phase, you need to notify all prescription and over-the-counter medications that you take to manage diabetes mellitus, hypertension, high blood lipids, and cholesterol, as well as other diseases and all vitamin and mineral supplements to your doctor. Your doctor will instruct you on medications you should stop taking by consulting you with another hospital specialist. Or a dose of those medications can be modified.
Since you will be sedated during the procedure, you will need a family member or a friend to drive you home after the procedure is completed and it is confirmed that your general health is stabilized. If it is impossible, you can seek help from healthcare professionals regarding your transfer to home.
Surgery and early postoperative period
After preparations, you will be transferred to the endoscopy room and positioned on the procedure table. Your doctor will administer a soothing agent, and thus, you will not feel the procedure. Sedative agents will help you relax and fall into a nap. Thus, the discomfort caused by the procedure will be minimized.
Your vital signs are checked throughout the procedure. Your throat is numbed as you may accidentally bite the endoscope, and your oral cavity is injured. A spray is used for this purpose. Moreover, a rubber mouth guard is placed to keep your mouth open.
The endoscope is then advanced into the esophagus through the oral cavity. After the mucosa of the esophagus is visualized, the structure and the tone of a circular muscular structure located between the distal end of the esophagus and the inlet of the stomach, called the sphincter, is evaluated.
The endoscope is advanced to the stomach, and the mucosa in all stomach parts (pylorus, antrum, corpus) is examined. If an ulcer is noted, it can biopsied or coagulated (burnt) with a device called cautery. Or, some drugs are injected into and around the ulcer to form scar tissue. If an abnormal growth of mucosa is seen, biopsy specimens can be collected before the lesion is completely removed.
Finally, the endoscope is advanced to the duodenum, the first part of the small intestines, and the endoscopic examination terminates; after examination, diagnosis and treatment are completed. The endoscope is removed, and you are observed in a room until the effects of sedation wear off. Before you are discharged, your doctor may make dietary recommendations and prescribe medications. You should strictly follow the instructions of your doctor to prevent risks and maximize comfort after the procedure. A family member or a friend should drive you home as you are administered a sedative agent. If it is impossible, you can seek help from healthcare professionals regarding transportation.
Distension, frequently passing gas, mild throat ache, and irritation are expected symptoms you may experience during and after an endoscopy. However, if you notice fever, shortness of breath, blood or black discoloration of stool, difficulty swallowing or feel insufferable abdominal pain, vomit, and see blood in your vomit, contact your doctor or visit the closest healthcare facility.
Results
All findings identified in the endoscopic examination are compiled in a report. If a biopsy specimen is collected, it will be examined in the pathology laboratory. Your doctor will inform you about treatment, precautions, and advice in light of all findings.




















